- Home
- About IAFP
- Membership
- Education
- Resources
- COVID-19
- Practice Management
- Adults & Seniors
- Behavioral Health
- Cancer
- Children & Teens
- Diabetes
- Health Equity
- Healthy Lifestyle
- Immunizations/Vaccines
- Infection Control
- Influenza
- Medical Cannabis
- Partner in Health Resources
- Obesity
- DIY Community Outreach
- Opioid Safety
- Physician Resiliency
- Rural Health
- Tobacco/Nicotine
- Advocacy
- Foundation
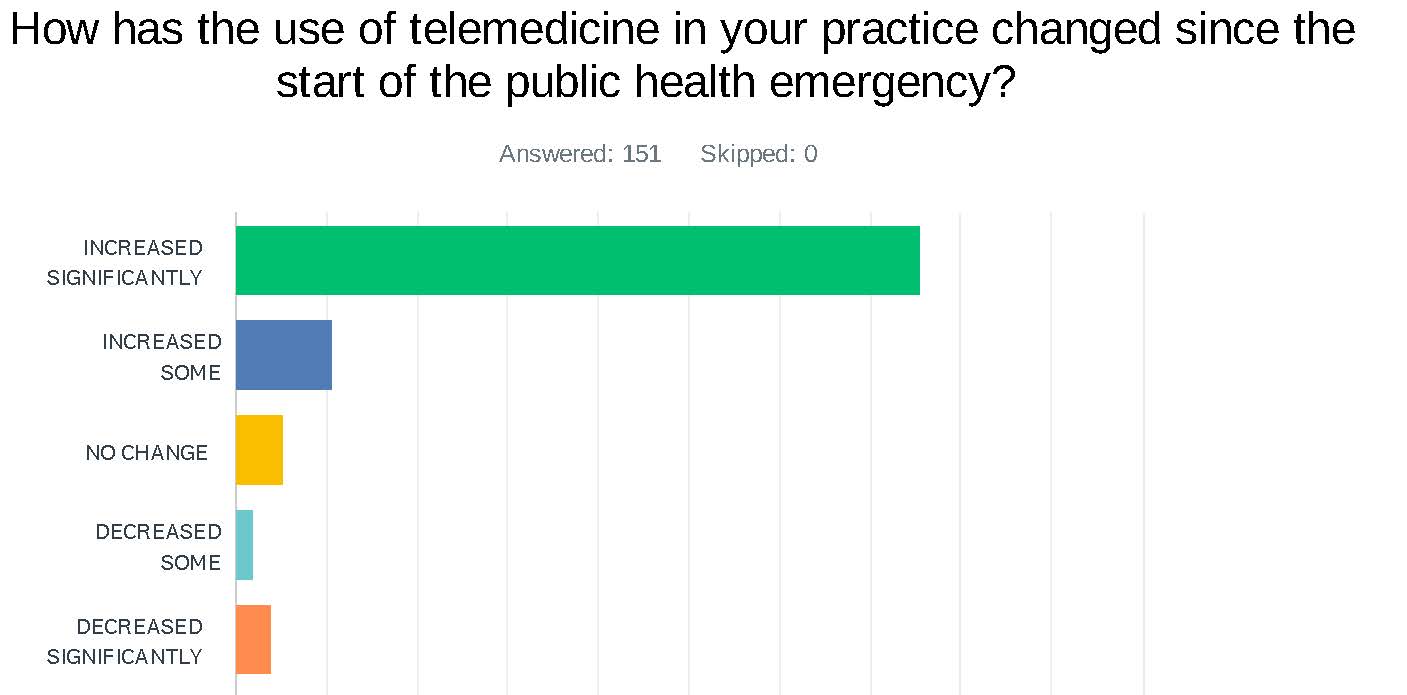
Statement on Telehealth - September 2020Governor Pritzker’s Executive Order 9 required that telehealth be covered by insurers no less restrictively than an in-person visit. It also prohibited consumer cost-sharing for telehealth services. The Illinois Academy of Family Physicians (IAFP) and the American Academy of Family Physicians (AAFP) believe this parity makes permanent sense. Impact on Family Physicians: Support from health plans to pay for telemedicine helped sustain family physicians who quickly deployed new technologies or updated existing capabilities to deliver telehealth services. Due to the COVID-19 pandemic, telehealth must be appropriately paid and is critical to ensuring adequate access to care for patients, the sustained health of communities, and the viability of comprehensive primary care practices. Even as practices resume in-person care, many patients may be reluctant to come for in-office visits until a COVID-19 vaccine is widely available. Also, the uncertainty around future waves of COVID-19 outbreak, which could lead to new stay-at-home orders, means that physicians need to be able to quickly pivot between providing in-person and virtual care. Physicians need adequate and stable telehealth reimbursement to continue providing virtual care to their patients. Impact on Patients: Patients with underlying health issues and the elderly continue to be at higher risk for developing serious complications from COVID-19. While these demographics are high risk for severe complications, the number of young and healthy people being hospitalized or worse continues to grow. The current financial situation will make it even more difficult for patients to meet their cost-share obligations. Telehealth offers a safe, cost-effective, and convenient means of caring for patients while reducing the unnecessary risk of transmission of disease to patients and health care staff. Many patients do not have the ability to pay the out-of-pocket costs associated with physicians’ services and may delay or skip essential health care.
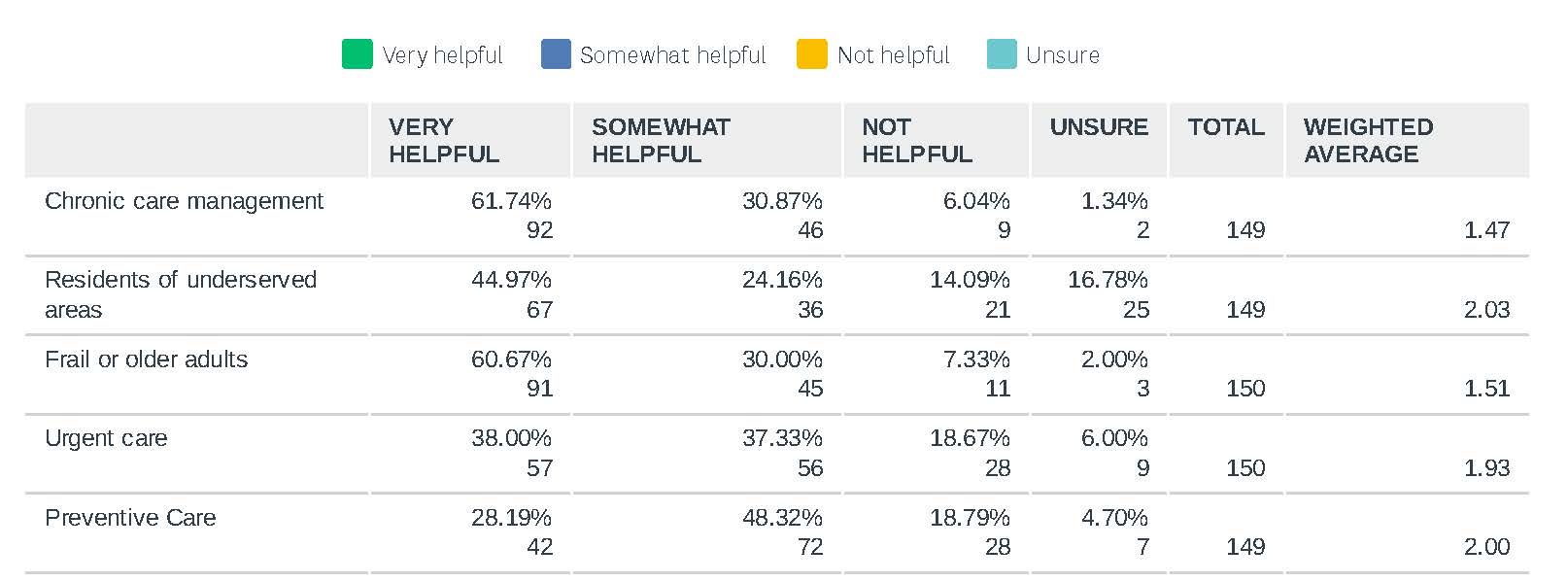
Adopt Medicare’s telehealth flexibilities for consistency and alignment to ease administrative burden for practices. Physicians do not differentiate between payers when seeing patients. Their priority is providing quality care to all patients, regardless of payer. As such we ask that Illinois insurers continue the following policies to maintain alignment with Medicare: It has become abundantly clear that telehealth contributes to comprehensive primary care. Research shows that patients with regular access to their primary care physician have lower overall health care costs and improved health outcomes. Physicians are able to get to know their patients in their home seeing things they may not have noticed in an in-person visit, contributing to better connecting patients to community-based services and other needs. IMPORTANT REASONS FOR OFFERING TELEMEDICINE IN IAFP MEMBER PRACTICES
Telehealth is a part of many methods to deliver care, not a standalone modality: Telehealth provides capacity to enhance and extend the four foundational dimensions of primary care: first contact, continuity, comprehensiveness and coordination. However, it should be one of many methods to deliver care, not the only one. The appropriateness of virtual care can vary based on a patient’s unique needs, something their primary care physician is best able to assess. Looking to the Future: The COVID pandemic has illustrated immense gaps in the Fee-for-Service (FFS) payment system. According to a survey, 82 percent of alternative payment model participants were able to leverage care management supports to manage their COVID-19 patients and others where only 51 percent of those in FFS were able to do the same. Telehealth can be a valuable asset for practices to improve patient engagement and enhance chronic disease management; and therefore, improve quality and lower costs through decreased disease morbidity. Telemedicine payments are a small part of a larger initiative, Marshall Plan for Primary Care supported by AAFP and IAFP to move primary care payment away from fee-for-service to a prospective payment model. On June 24, BlueCrossBlueShield of NorthCarolina stepped boldly forward to shore up independent primary care practices in the state and help them move into value-based payment arrangements. We strongly urge all payers to: |